Aelin's Birth Story: Why I Have Postpartum PTSD
This has been the hardest blog post I’ve ever written. I do not want to be this vulnerable, much less with the masses, but so much about what happened to me when I gave birth to my precious girl was not okay and I need to draw attention to it. If nothing else, so that other women who have experienced similar treatment know they’re not alone, that what happened to us was not okay, and to hopefully start a dialogue that will prompt changes to take place. While there were many, so many, things that happened during my and Aelin’s hospital stay that were atrocious, no one has time to read a 50 page novella, so I’ll only hit on the most egregious points. Without further ado, here is Aelin’s birth story:
BA: Before Aelin
Leading up to her birth, I tried to be prepared. I had my bags packed months in advance, I had talked to my OB about my past trauma and all my concerns, the few things I was just not willing to consent to, while still recognizing I was not in control. I told many people I was hoping for an unmedicated, vaginal delivery but was not going to lock myself into saying I wouldn’t have an epidural, and I recognized there was a chance I would need a C-section. I was nervous but optimistic that even if things didn’t go according to my plan, I would still find the beauty in her birth. What I received was worse than my most intense, hormone fueled nightmare, and I struggle to find any beauty in the experience.
Two days before Aelin was born, all was well. I was tired and felt like a beached whale, but I was out getting my maternity photos taken. After we returned home, I was standing by the counter peeling potatoes for dinner when suddenly there was a huge gush of water that soaked my panties, ran down my leg, and puddled on the floor. My water had broken, but Josh and I were in a state of in denial; neither one of us wanted to go to labor and delivery because of the awful experience we had in January when I had premature labor, but when I started throwing up we knew it was for real, so we grabbed the bags and left. At L&D they told me I peed my pants, didn’t even ask me to pee in a cup, and sent us home.
The whole next day I did not feel right, but Josh said if we went back to L&D that we would just get brushed off again, so I slept and tried to calm the feeling of unease I had.
The next morning I got a phone call from Maternal Fetal Medicine. Because I have diabetes, I had been seeing a doctor there, whom I adore. My doctor there was concerned about the lack of tests run two days prior and asked me to come to her office. Josh and I both texted our bosses and headed straight there. After putting me on the monitors for awhile and ordering a urinalysis and blood work, my doctor at MFM told me my blood pressure was really high (that had been low my entire life and entire pregnancy until this point) and asked me to go to L&D to be monitored while we waited for the labs. I texted my doula and asked her to meet us there.
At labor and delivery I was admitted and they monitored my blood pressure which was staying high. They wanted to put me on magnesium sulfate (which I did not know at the time has many scholarly articles that state there is a strong correlation between mothers who are given it and NICU admittance for lung issues) and when I asked what the side effects where, the response I got was “none.” I had an extreme adverse reaction to this medication. After my blood pressure came down some, I was told I had only two choices: they could induce me and give me 24 hours to see if I could deliver naturally like I had hoped, or I could just opt for a C-section. My doula pointed out that magnesium is used to stop contractions so if they were going to give me Pitocin to induce labor, the magnesium would work against the progression of labor, and the nurse admitted that was true. Josh asked if there were any other options we could try to keep Aelin in longer and they said “no.” No discussion, no explanation, no offering me the steroid shot for her lungs and keeping me there even just 12 more hours to give her a chance, since they were already okay with giving me time to labor, just no. I have since talked to friends who are labor and delivery, NICU, mom and baby nurses, as well as a midwife who have said this is not normal; at their hospitals there are more options discussed than just the two they handed me. Because the doctor that would be on call the next day was one I do not like because he told me in January to think of the fibroid on my uterus as “the dead twin” (not something you say to any woman, much less one who has experienced miscarriage), and I was told if I did a C-section that day that my OB would come in and do it, I opted for the C-section.
Everything moved very quickly at that point. My doctor came in twice and chatted with us, not about anything really important, but I appreciated it at the time.
I was taken in a wheelchair to the OR, and not long after, I heard Aelin's first cry. I smiled hearing how strong it was, even my OB commented that she was “sassy.” Then everything turned upside down.

Aelin’s Arrival
A few minutes later, they took a rosy colored Aelin right past me. A nurse paused for all of two seconds to curtly say “we’re taking her to the NICU” and then my baby was gone. I had told Josh months prior that in the event something were to happen that would require Aelin to need the NICU, he was to leave me and not let her out of his sight. I could speak and consent for myself, she could not, so he needed to be with her. So I laid there, alone on the operating table wondering what had just happened while no one explained anything to me. I couldn’t even see anyone behind me, and my OB chatted with his assistant about travel plans while he stitched me up without a word to me.
The following is a letter I sent to the Utah Hospital Association and every email I could find for the administration at the American Fork hospital:
On April 25, 2022, I gave birth to my daughter, Aelin Hansen, at the American Fork hospital via C-section. The actions and attitudes of several nurses and doctors during that experience has left me with postpartum PTSD. Specifically, nurse practitioner ____ was extremely unprofessional, bullied me and my husband, lied to my husband and my mother about a procedure for my daughter, and committed HIPAA violations.
I was told by nurse ___ that before Aelin was even delivered, NP ____ told her she was going to admit my daughter to the NICU, “…because the mom is a type 1 diabetic.” I am, with an A1C of 5.1; my daughter’s blood sugar at birth was in normal range, although I was the one that insisted they check her glucose levels, because they hadn’t. Until the evening of April 23, my pregnancy had no complications due to diabetes; in my last appointment with Dr. Feltovich, my MFM doctor, she told me she would see me at 38 weeks and we would decide how to proceed then. There was nothing indicating a problem with me or Aelin. It is not acceptable to decide to admit a baby to the NICU before a problem is known.
The NP was unprofessional in her interactions with me, and had absolutely no bedside manner. When I was being moved from labor and delivery to my room, I was taken to the NICU. Keep in mind, at this point, I had not so much as been allowed to touch my daughter. So, I began to ask Ms. ___ questions, because I wanted to know what was wrong with my baby; no one, to that moment, had explained why she was taken straight to the NICU. I heard her loud cry in delivery, and even Dr. ____ commented on her being sassy. There had been no indication as to what was wrong. Every question I asked Ms. ____ was dismissed. She acted annoyed that I was even asking questions, trying to understand, even though Intermountain’s own Children’s Bill of Rights states that parents have the right to be a part of the child’s care team and informed of what is happening. I asked how long she thought my daughter would need to be in the NICU, and her response was, “plan on maybe her being out by your due date.” This was April 25, and my due date was May 29. She made that statement without offering a reason – apparently her decision did not require explanation, or at least not to us, Aelin’s parents. In that moment, right out of surgery, unable to walk because of the effects of the anesthesia, and not knowing what was wrong with my baby, a baby I had still not been allowed to hold, the callousness in her estimation of when Aelin would be able to go home was incredibly distressing.There was no kindness or compassion in her demeanor. She then told me they would be giving Aelin a preventative antibiotic (what they were trying to prevent, I’ve never been told) and I said I wasn’t comfortable with giving her an antibiotic, as a prophylactic. I, and other members of my family, have a long list of antibiotic allergies, and I was concerned that Aelin might have inherited the same. Ms. ____ told me that babies cannot have an allergic reaction for the first year. I asked if that was the case, why, in doctor’s appointments for 1- and 2-month-old infants, are parents asked about any allergic reactions to medications? She did not answer my question, instead resorted to fear tactics and bullying, telling me that my daughter could die if she needed the antibiotic and didn’t already have it in her system.
I was taken to my room, but pushed myself to return to the NICU; I did not feel my child was safe because of Ms. _____’s calloused attitude. My nurse wheeled me back to the NICU after a few hours, because I was so concerned about my child. I was pleasantly surprised when the nurse in the NICU asked me if I wanted to hold Aelin. Within a second of her being placed in my arms, for the very first time, Ms. ____ barged back into the room. She saw me holding my daughter, and did not give me and my spouse two minutes to enjoy that precious moment. She asserted that Aelin needed the antibiotic, right then, again launching into a several minute tirade about how she could die if it wasn’t given, ending with,“What do you think?” I responded, “I’m going to be very candid; I am just now getting to hold my daughter for the first time, at the end of a very hard day, I don’t have the mental or emotional bandwidth to give you an answer right this second.” Ms. ____ raised her voice, stating that time was, “of the essence,” and she would give us a few minutes, but would be back with a paper for us to sign, refusing the antibiotic, and she stormed out; incredibly unprofessional. This antibiotic was supposedly a prophylactic, not an anti-seizure medication or a similar medication, and she did not, and would not explain the urgency. All we wanted was five minutes, to have that moment, my husband and I, with our daughter, as a family, and Ms. ____ showed no compassion. At that point, I told my husband I needed to go back to my room because the stress of Ms. ____’s bullying, on top of everything else (the C-section and the meds, including one that caused an adverse reaction) had me near the point of passing out, so my husband stayed behind to deal with the antibiotic question.
My husband, who is non-confrontational, was extremely uncomfortable with Ms. _____’s demeanor. He called my mother, put her on speakerphone and directed Ms. ____ to answer her questions regarding the antibiotic. My mother brought up a concern for Aelin’s microbiome being damaged by the antibiotic. Ms. ____ acknowledged the validity of that concern, and told both my mother and my husband that it was routine at IHC to administer a probiotic and a prebiotic with the antibiotic. At that point, my husband said, if they would give her a probiotic and a prebiotic to protect her gut health, then he would consent to the antibiotic. When he told me later that night he had made that decision, I was at peace with it. However, Ms. ____ lied to him and my mother and never put in the order for the probiotic or the prebiotic. He consented ONLY if those were given and they were not; she administered an antibiotic to our child without our consent. Now Aelin is dealing with stomach issues, because her gut bacteria was damaged by the antibiotic that Ms. _____ gave, without a probiotic and prebiotic.
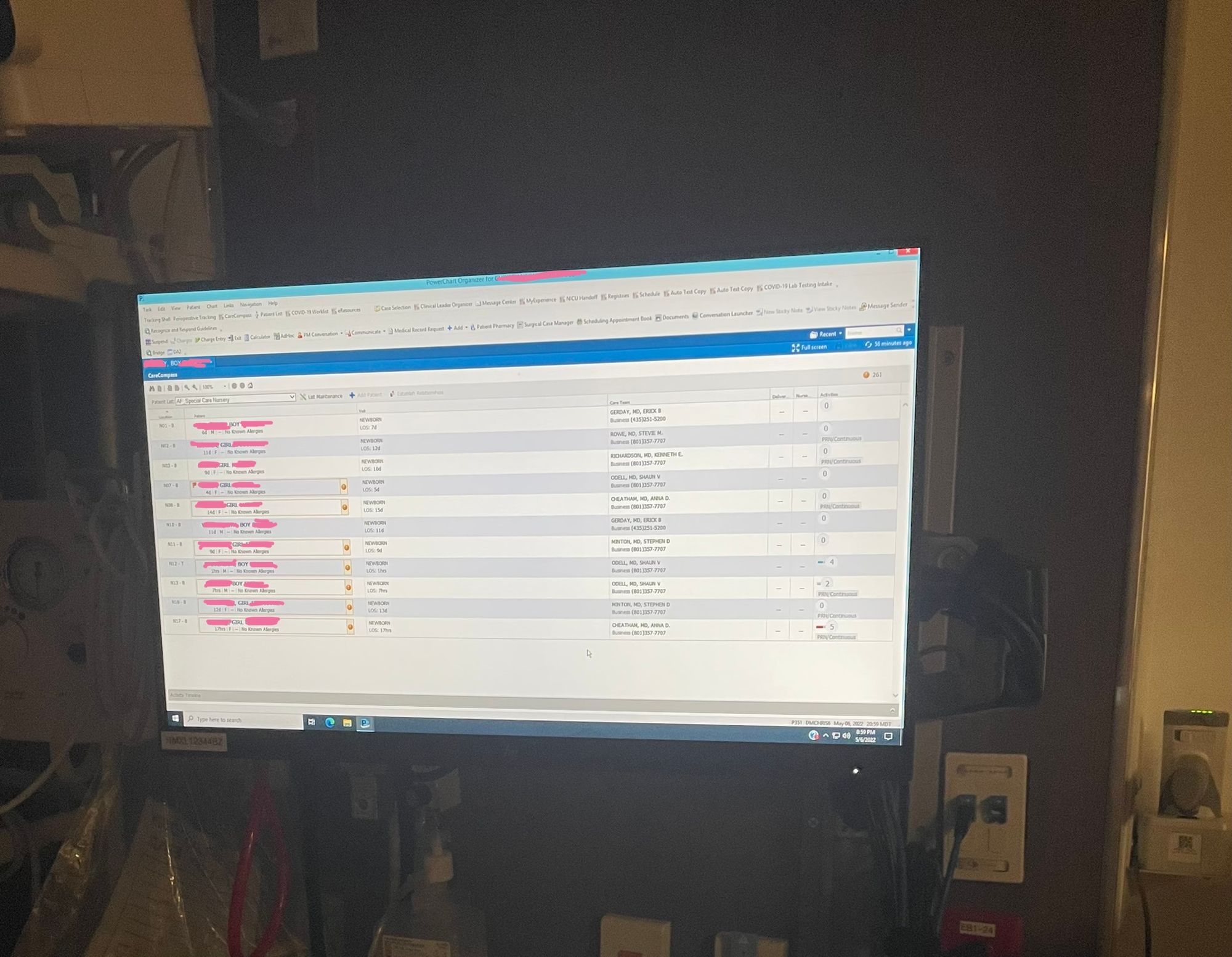
Ms. ____ also logged into the computer and left it up when she left the room, giving us access to all the babies’ charts in the NICU. That is a major HIPAA violation, one we saw committed by many nurses, time and time again. Additionally, I have pictures of the computer screens, showing all the patient names as proof, though it is my understanding that one of the photos I took of the screen may have already been given to nurse administration, since I have an acquaintance in the hospital with whom I shared this.
Personally, I feel assaulted because of the actions of some of the nurses and doctors who were supposed to provide care to me. According to Dr. ___, my sexual trauma is supposedly clearly stated in my records, which makes some of the behaviors even more disturbing to me. However, I am most upset by the bullying, HIPAA violations, and proceeding with a treatment, without consent, by Ms. _____. I hope she is stopped before she causes damage, emotional or physical, to more mothers and children
American Fork hospital still has not responded.
The next morning, we got a phone call to the landline in my room that Josh answered since I couldn’t reach the phone from my bed. It was the NICU telling us they were going to do an X-ray on Aelin. Not asking for consent, not explaining what they were X-raying or what they were looking for or why, telling us they were going to do something to our child. Josh said to wait, he wanted to be there for it and hurriedly put on a shirt and headed straight down, only to find that they were not going to wait, he made it just in time to be present for the X-ray. After that, a different nurse practitioner told him that the X-ray found Aelin had a little bit of fluid in her lungs and tried to scare tactic him. He asked her to come back to my room and share that information with me. He walked in looking panic stricken so when the NP told me she had fluid in her lungs and that was all, I was confused going “yeah so? A lot of babies do after they’re born” to which the NP tried to tell me a long list of what could go wrong before leaving my room.
I learned later that morning when asking why Aelin had a gigantic bruise on her head, and what looked like a slight black eye, that my OB had vacuumed her out. When I had met with him in the months leading up to her birth, I had told him in the event of a vaginal birth, I was not okay with an episiotomy due to my trauma (mentally, I would rather tear than be cut) unless it was a choice between an episiotomy or her needing to be vacummed out, in which case, cut me as far as needed. I was not okay with a vacuum due to the risk of brain damage. I had no clue that they used vacuums in C-sections and feel this would have been an appropriate thing for him to have discussed with me and Josh one of the two times he came in my room before the surgery. At 6 weeks old, Aelin still has burst blood vessels above her eye where she was suctioned out, despite me saying I would not consent to the vacuum, yet we were never told why. We’re just her parents, after all.
Around this time, they also started Aelin on poly-vi-sol with iron without my, or Josh’s, consent or even telling us. Josh just happened to notice them putting it in the feeding tube one day and asked what it was. Poly-vi-sol with iron can be purchased over the counter (though, we were given a prescription for it when discharged) and says on the packaging it is for babies 4-6 months of age as they transition to solid food, not newborns on breast milk (and her iron was in normal ranges based on the labs they took but never reviewed with us). The one time we gave her poly-vi-sol with iron two weeks after we got her home, it caused several adverse reactions (things that happened in the NICU and they used as reasons they needed to keep her there) that made her pediatrician tell us to not give it to her again, only after the first time, I had already thrown it in the trash where it belongs.

Lack of consent didn’t just apply to Aelin. A few days after she was born, my blood pressure was still acting up. Per one nurse’s request, I returned to my room at a specific time so she could take my vitals (because apparently it’s a big ask for her to walk down the hallway to the NICU and do it there so I could be with my baby like a few other nurses later did) and found my blood pressure was pretty high. She told me to “stay put” while she called the doctor on call. I told her we had an appointment in the NICU at 2 (it was 1:30), so if she wasn’t back by 1:50, she could find me in the NICU. She told me I needed to stay in bed and I told her that wasn’t happening. Shortly after 2, Josh and I were in the NICU waiting on lactation when the nurse wheeled a blood pressure monitor down, looking pissed. She angrily told me “your doctor wants you in bed.” I replied “well good thing there’s a daybed in here, then.” Then she said that if I didn’t return to my room she would have them “put me back on mag” (a medicine I told her earlier I needed to add to my list of medications I’m allergic to because of how sick it made me). I reminded her that she, and no one else in that hospital, had a right to put me on, or do anything, that I did not consent to. She somewhat backed down at that. However, her threat over my bodily autonomy induced a trauma response and my blood pressure climbed even higher. Their solution for this was to tell me I needed to be in my room, away from my baby who was with people I did not trust because of their treatment of us; they thought that would somehow help. I refused and stayed with my baby, where I belonged.
By the third day I was in the hospital I had stopped bleeding and was thrilled because the nurses and doctors checking my bleeding was a really triggering experience due to my history of sexual assault. I knew I needed to try to work through it while I was bleeding, but now that I wasn’t bleeding, there was no reason for them to check and see if there was too much blood. I was so happy that part was over. Wrong. Every time a nurse or doctor would come in, they would ask how my bleeding was and I would respond that it had stopped and told them to not check. I might as well have remained silent because without fail, they would still pull my pants down without a word to me. The last doctor who did it asked if he could check my incision to which I said “yes, but do not check my bleeding” and he pulled my pants down anyway. I cannot think of any scenario in which a person says “do not remove my pants” and another person wordlessly does so anyway that would not be classified as assault. Yet for some reason, doctors and nurses believe they function outside the laws.
The Aftermath
We know that rape and assault have nothing to do with sex and have everything to do with power and control. The doctors and nurses at American Fork Hospital constantly and consistently took away any power or control I had over my own bodily autonomy. When I tell you that that has not been good for my mental health, it’s the understatement of the century. 1 in 3 women experience some form of sexual assault in their lifetime, so even if they’re not as vocal as I was (for all the good it did me) with my OB leading up to delivery about how important consent is to me, you would think that a group of providers who deals exclusively with women and babies would be mindful of that statistic, and tread carefully. You never know what the experiences of the person you’re treating might have been. Is it any wonder postpartum depression and maternal mortality rates are on the rise with this sort of behavior?
On the topic of postpartum depression, I was constantly bombarded with the postpartem depression questionnaire in the hospital. The first night, I glanced at it and knew I couldn’t fill it out. Every morning and every night, I had a nurse badger me to fill it out, and every time I replied the same way “I can’t fill this out. I can’t look inward or be introspective at all right now or I’ll fall apart. I have to keep looking forward. It’s like in the third Harry Potter movie, how he has the Monster Book of Monsters, a book that flies around and destroys everything unless he keeps it belted shut, I have to keep my feelings and emotions belted shut right now.” One nurse simply replied “well if you don’t fill it out tonight, I’m just going to nag you in the morning” to which I said “fine, I’ll just tell you the same thing come morning." No care, no concern, they just wanted me to check their box. Like Josh said to a nurse practitioner, “doesn’t the fact that she can’t even fill it out tell you everything you need to know?” To which I would say that it probably would tell them a great deal if they actually cared, but after everything that happened to us there, it's quite clear they do not.
Aelin made it out of the NICU just shy of 2 weeks, which I believe was because of the constant vigil Josh and kept in her room, making sure she was getting the things she actually needed and things the doctors ordered that half the time the nurses just didn’t bother to do. She was released on a Saturday and by the following Wednesday, when we took her to her pediatrician, she had gained almost a whole pound. Amazing what happens when mom and dad are actually allowed to feed their baby when she indicates she’s hungry and not just when the nurses will allow. A few days later, Aelin was off oxygen. She is thriving in a home environment, even though according to that awful nurse practitioner, we should only have been allowed to bring her home maybe 9 days ago at the earliest.
If Josh and I ever have another baby, and it’s a pretty big if at this point, I will not give birth in a hospital. I am so traumatized that I will risk a home birth before going back because that seems so much safer and less emotionally damaging than going through even a fraction of what we experienced at American Fork.
I do not believe all nurses and doctors are horrible. There were a few nurses that, when we were discharged, we left thank you cards with gift cards to Starbucks and Dutch Bros and even had a cute, pink gift basket in Aelin’s room. There were a couple beautiful souls that on the days and nights they cared for Aelin, Josh and I went home and got a few hours of sleep because we knew Breezy, Lisa, Shannon, and Beata would do everything in their power to make sure she was taken care of. However, they’re the exception, not the rule. In my experience, the Breezys, Lisas, Beatas, and Shannons are in short supply and the nurses like the one who threatened me, and another who raised her voice at Josh for having the nerve to ask questions, abound.

Healthcare in the US, especially where women and babies are concerned, has to change, and American Fork hospital has a lot of change that needs to happen just to make their treatment of women humane. Postpartum depression and maternal mortality rates are on the rise, and a huge contributing factor to that is the bullying, lack of consent, lack of informed consent, and overall lack of care women receive when going to a hospital to give birth; arguably the most vulnerable position she will ever be in.
To my friends and family who didn’t understand my silence the last 6 weeks, now you know why I dropped off; I’ve been traumatized and processing. But, you know me, when something really bad happens to me, I have to do my part to stop it from happening to someone else. I don’t want any other woman or family to endure what I did; what should have been one of the happiest days of my and Josh’s lives instead is one of the darkest. American Fork hospital and Valley OBGYN, do better.
UPDATES:
June 10th, 2022: I just spoke with a patient advocate at IHC who was concerned at my use of the word “assault.” When I referenced my blog her words were “well I read in your blog where they pulled your pants down after you said not to, is that what you’re referencing?” And then went on to say as part of their assessment, they’re required to notate color and amount of blood. My response to her was I said not to do it, I have a right to refuse something, and if I say don’t do something, they do not have the right to just wordlessly do it anyway, otherwise it is assault.
The fact that they don’t understand this concept makes me skeptical of any changes being made.

